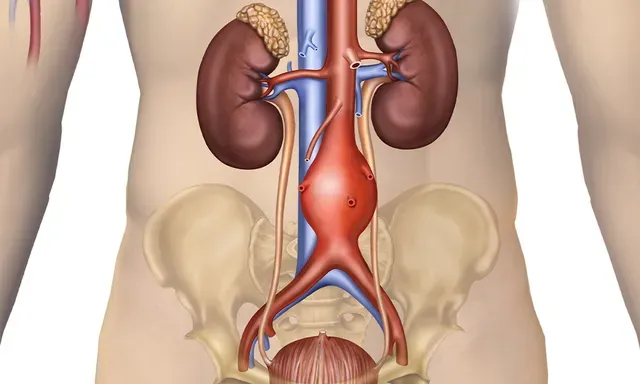
Abdominal Aortic Aneurysm (AAA)
Every year in the United States, about 200,000 people are diagnosed with an abdominal aortic aneurysm (AAA), a balloon-like swelling of the main artery that supplies blood to the lower body. Left undetected and untreated, an AAA can rupture and cause life-threatening bleeding. Vascular surgeons, Drs. Danón Garrido, Justin Manley and their first-rate team at Advanced Vascular & Vein Associates in Flowood, Mississippi, offer comprehensive care for patients with AAA from the Greater Jackson area. Call today or book an appointment online any time.